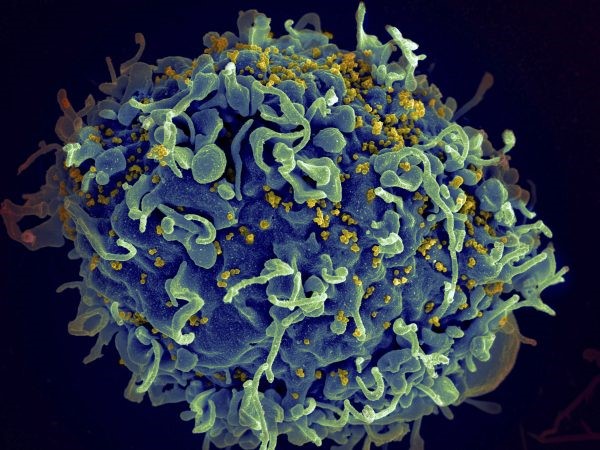
Human immunodeficiency virus, or HIV — the infection that can damage the immune system and lead to the deadly disease AIDS — hasn’t been in the news as much as it was during the beginning of the AIDS crisis in the 1980s. Still, an estimated 1.3 million new HIV infections were reported around the world in 2023, with 630,000 related deaths, according to the World Health Organization.
Related Articles
Biden health officials say they built up US pandemic defenses. Trump promises changes
Opinion: Whooping cough vaccine has an awareness problem
Is bird flu the next pandemic? What to know after the first H5N1 death in the US
5 things we know and still don’t know about COVID, 5 years after it appeared
Flu and RSV are sustaining California’s sniffly season, COVID yet to surge this winter
Anti-viral treatments for HIV have helped reduce the number of AIDS-associated deaths, and the new HIV infections in 2023 were down from 2.1 million in 2010. But there is no cure for HIV or AIDS or a vaccine for human use to prevent infection.
One of the labs involved in current research to design such a vaccine is at La Jolla-based Scripps Research, which recently made a discovery that could drive development of the vaccine.
Many vaccines work by introducing a protein to the body that resembles part of a virus. Ideally, the immune system will produce long-lasting antibodies recognizing that virus, thereby providing protection.
But Scripps Research scientists said they have found that for some HIV vaccines, something else happens. After a few applications, the immune system begins to produce antibodies against immune complexes already bound to the viral protein.
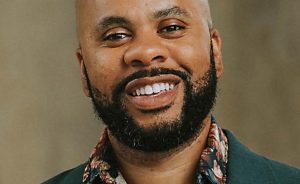
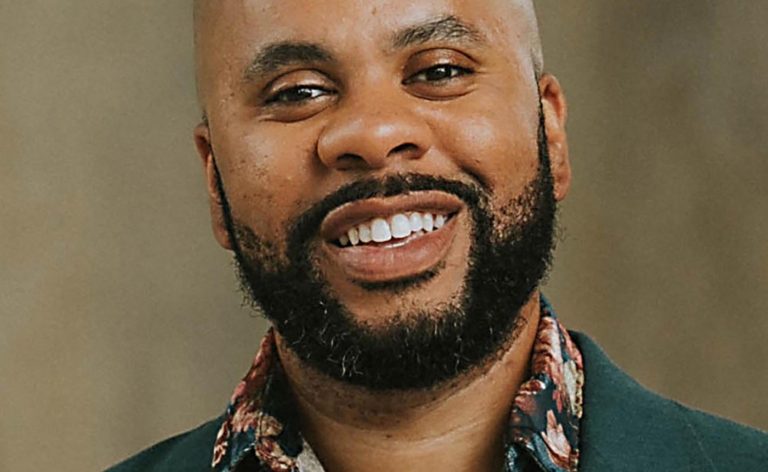
“It’s a unique reaction in which antibodies bind to other antibodies, which is rare,” said Scripps researcher Sharidan Brown, first author of a study published Jan. 17 in Science Immunology. “Over the course of multiple immunizations [in animals], we have found four classes of antibodies that cling to other antibodies. They are unique responses, so by understanding the structure for the first time, we are put on the right foot to understand these better and can harness them for not only HIV vaccine design but other therapeutics.”
The observation came about when researchers in the lab of Andrew Ward, a professor of integrative structural and computational biology at Scripps Research, was using advanced imaging tools to study how antibodies evolve after multiple HIV vaccine doses. A technique the lab invented, known as Electron Microscopy-Based Polyclonal Epitope Mapping, or EMPEM, let the researchers see exactly where on the virus antibodies bind.
When they carried out the experiments on blood from animals that had received multiple doses of an experimental HIV vaccine, they discovered that some of the antibodies were not binding directly to the HIV viral antigen but to immune molecules on its surface.
It isn’t yet known whether this binding is a good thing in designing an effective vaccine, but Brown said future studies should answer that question.
“It adds to our understanding of what these vaccines are capable of eliciting,” Brown said. “We don’t fully know what these antibodies do yet, but by understanding and future experiments looking into why they get elicited and what they do, we can adjust vaccine studies to make them more effective by either harnessing or getting rid of it.
“It could be a good thing [that the antibodies bind together] because it could give the immune system a bigger set of antibodies. Or it could be detrimental in that it is not making antibodies the body needs.”
She and others in the lab “are excited to see where these antibodies fit into the immune response and the body’s ability to fight off HIV,” she said. “This could lead to redesigning vaccines to target or eliminate these responses and could lead to better vaccines.”
Implementation of any vaccine stemming from this discovery is years away from human trials, but Brown said an effective vaccine would have a great impact.
“There are still millions of people diagnosed with HIV, so having a vaccine would impact the lives of people around the world,” she said. “Having a vaccine that prevents infection would be instrumental in reducing the spread. Right now, there are no vaccines in use in humans. There are clinical trials in humans, which is exciting, and we have made a lot of progress toward eliciting the types of antibodies with these vaccines in the past five years or so. This [discovery] is an extra data point to think about when we design these vaccines and could help us better design boosting immunizations.”
Brown, a native of Montana, “where I fell in love with science,” said she came to Scripps Research for her Ph.D. studies and was placed in her current lab to research immunology and structural biology.
“I feel super lucky to work in the lab I do,” she said. “We have such a diverse, large lab of people full of amazing ideas.”
The next step for the lab is to look at the antibody responses in other models.
“We want to understand how they are generated and what they do, and any consequences to these antibodies being around,” Brown said. “Then we can modify these types of responses in vaccine design.”