This fall, prepare for the latest round of COVID vaccine Whac-a-Mole. Like the old arcade game, no matter how many shots we get, the enemy always pops back up.
But here’s why the new shot, recommended by FDA advisers last week, makes sense: It targets a new version of the virus, the FDA panel said. It bolsters your body’s ever-growing defense system. And it’s a lot better than getting very sick or hospitalized.
Last year’s shot isn’t holding up. Protection against both infection and severe illness is waning.
“Effectiveness has decreased, as the time since vaccination has increased — and as new SARS-CoV-2 variants emerge,” said biostatistician Danyu Lin of the University of North Carolina School of Global Public Health, who presented worrisome new data to the FDA advisory panel.
The old vaccine’s effectiveness peaked one month after the shot, Lin’s team found. After four weeks, the vaccines were 52.2% effective at preventing infection and 66.8% effective at preventing hospitalization. After ten weeks, effectiveness at preventing infection decreased to 32.6% while effectiveness at preventing hospitalization decreased to 57.1%.
By comparison, the Centers for Disease Control and Prevention says that with the annual influenza shot, “during seasons when flu vaccine viruses are similar to circulating flu viruses, flu vaccine has been shown to reduce the risk of having to go to the doctor with flu by 40% to 60%.”
Last Wednesday, FDA’s advisers, a panel of physicians from hospitals and universities around the nation, unanimously voted to recommend a new vaccine. Vaccine manufacturers Pfizer and Moderna say they were prepared to make updated vaccines available in August, pending final FDA approval. As in previous years, the U.S. Centers for Disease Control will make specific recommendations for the elderly, immunocompromised, youth and other groups.
The new vaccine will target a variant of the ever-evolving coronavirus called JN.1. Last year’s vaccine was based on the XBB lineage of the virus.
Fortunately, the COVID virus isn’t changing in a way that would make it a serious threat to most people — turning it into something far deadlier, such as Ebola. Each new version is a subvariant of the omicron variant that first appeared in 2021 and, though highly transmissible, hasn’t proven to be particularly virulent.
But it is drifting in smaller ways, complicating our vaccine strategy. The original virus first detected in Wuhan, China, was replaced by the alpha variant, which was replaced by the delta variant, which was replaced by the omicron variant. A subvariant called BA.1, then BA.2, became the most common circulating versions of omicron.
Since then, the virus family has continued to multiply and diversify. There’s an evolutionary arms race — as the immune system makes new antibodies, the virus develops new mutations. Each iteration seeks to offer some sort of advantage, such as an ability to sidestep the immune system or extreme contagiousness.
Late in 2023, variant JN.1 overtook the XBB lineage.
There’s a wrinkle in the new vaccine strategy: By next fall, JN.1 may not be the dominant virus. Already, a subvariant called KP.2 is on the rise. But the new vaccine formula likely will be effective against both strains — and, because manufacturing takes time, a decision must be made now.
When compared against results from the original shot, the benefit of the new shot may seem modest. That’s because the original vaccines were given to a completely unprotected population, with high risk of hospitalization and death, said Lin. Now, with four years of inoculations and infections, the general population has a wide range of vulnerabilities.
While the vaccine is free to both insured and uninsured individuals, this cost is still real. The federal government paid, on average, $20.69 per dose, and the cost of the new vaccine is likely to be higher. But vaccines save money by preventing hospitalization, lost productivity due to illness and potential Long COVID.
Related Articles
Abcarian: Republicans would rather demonize Fauci than help Americans survive next pandemic
Positive test not needed for long COVID diagnosis, experts conclude
How much are student absences costing Bay Area schools?
Ex-East Bay IRS officer, five others sentenced to prison for COVID-19 fraud scheme
San Jose, Oakland airports await summer as passenger rebound stalls
Research is now underway to create a universal vaccine that works against all strains of the virus.
Powerful combination vaccines are on the horizon, easing the chore of multiple shots. On Monday, Moderna announced that, in a Phase 3 clinical trial, its combination COVID and influenza vaccine generated stronger immune responses in older adults than individual vaccines targeting those viruses individually. A combo shot could be on the market as early as autumn 2025.
The FDA news comes as Americans are vaccine-weary and increasingly indifferent. The Centers for Disease Control and Prevention estimates that, as of March, a mere 28% of American adults have been vaccinated with the latest vaccine. Why bother with another shot? Medical experts say there are still many reasons to get the jab:
• Protection from previous shots, especially the primary series, has waned — so some people are getting very sick. Research shows that a large percentage of those hospitalized for COVID-19 had been vaccinated with the primary series but hadn’t gotten an updated shot.
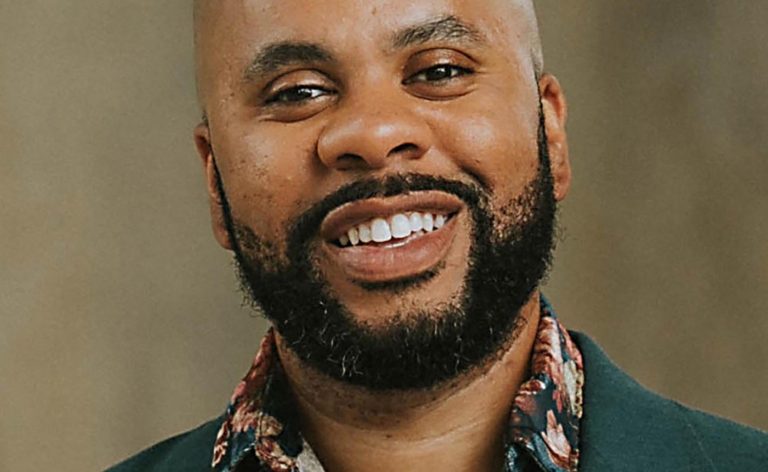
• Each additional shot helps. There is evidence that each vaccine or infection, especially in the first few months after receipt, provides added protection against critical illness and hospitalization. “Through multiple immunizations, your repertoire of immune cells expands,” said Jeremy Kamil, a virologist at Louisiana State University Health Sciences Center Shreveport, who studies variant mutations. “Your body learns to make these very potent antibodies that are active against multiple strains of the virus, so it becomes harder for the virus to wiggle away from them. … You’re much better defended.”
• If you get infected, it will likely be less severe. Think of seatbelts and airbags — they don’t prevent car crashes, but they boost your chance of survival. Similarly, COVID vaccines are not 100% protective, but an immune response will be more vigorous, so your illness will likely be briefer. Furthermore, research shows that vaccines help protect against Long COVID.
• Vaccines are easier on your body than infection. A sore arm and perhaps body chills are better than days of illness and perhaps hospitalization. “You’re setting yourself up for success the next time you see the virus,” said Kamil. “Your immune system will say, oh, I gotcha. I know who you are.”