You’re less likely to die of cancer today than you were a generation ago.
True, you could’ve said the same thing 20 years ago and 40 years ago. But the gains made against cancer during the first two decades of the 21st century are so profound – and so unexpected given other trends that should be leading to more cancer deaths, not fewer – that some experts are talking again about the idea that cancer could be cured.
The Centers for Disease Control issued a report in June that crunched a range of U.S. cancer statistics collected during the first two decades of this century. The data track how roughly two dozen types of cancer played out in hundreds of locales, and they measure disease outcomes for all Americans based on gender, age and race.
It’s a complex study, but the bottom line is simple:
Cancer isn’t as lethal as it used to be.
In fact, the report’s key finding is that the U.S. cancer death rate was about a third (29.2%) lower in 2022 than it was in 1999.
“I don’t know if I’d have had the same outcome if I’d been diagnosed 20 years earlier, or even six months earlier,” said Tasha Champion, an Apple Valley resident who was diagnosed with an aggressive form of breast cancer in 2016, a day before she turned 36.
“I can’t say if cancer treatment, overall, has changed. I wasn’t involved in it before. But I’m glad to be where I am now, which I’m positive is because of the treatment I got at the time,” she said.
“A lot more people, like me, seem to be winning.”
Like much of the CDC report, the death rate, which strips away population growth, is a number that tells a very human story. At the turn of the century, cancer was killing 200.7 out of every 100,000 Americans, but by 2022 the number was down to 142. In a city the size of Burbank (population 104,000) that translates to about 60 lives saved per year. In a nation the size of the United States, population 333 million, that translates to about 3 million lives saved since 2000.
The agency also looked at the geography of cancer, tracking trends by state, county and even congressional district. In California, cancer deaths are running about 10% lower than the national average and the state’s gains in cancer mortality since 2000 match the gains made nationally.
County-level cancer numbers in the report cover only a five-year window ending in 2022, so it’s tough to track long-term trends. But, locally, those numbers also paint a mostly upbeat picture. People living in Los Angeles, Orange and Riverside counties are all less likely than other Americans to die of cancer, and the cancer death rate in San Bernardino County is within the margin of error for matching the national average.
All of which isn’t to suggest the story of cancer in America is only about numbers.
Oncologists and other experts and even some patients, like Champion, say every gain against cancer has involved some combination of human tenacity and intelligence and imagination. That formula, they add, can be applied to everyone from lab-bound researchers to patients volunteering for clinical trials.
And just as cancer isn’t a single disease (but is, instead, a constellation of diseases in which the bad actor cells tend to behave in a similar fashion) experts note there’s no single reason why the fight against cancer is going well.
For that, they point to changes and advances and trends that range from the obvious to the obscure.
The anti-smoking campaigns of the 1980s and ’90s are paying off in fewer cancer deaths in the 2000s. And while the Human Genome Project, which launched in the 1990s, didn’t lead to a cancer cure, as was once suggested, it did spin off other research that translated into DNA- and RNA-based ways to detect and treat many common types of cancer.
Even new laws – hikes in tobacco and alcohol taxes and municipal codes that limit the use of tobacco in public places – have led to fewer cancer deaths.
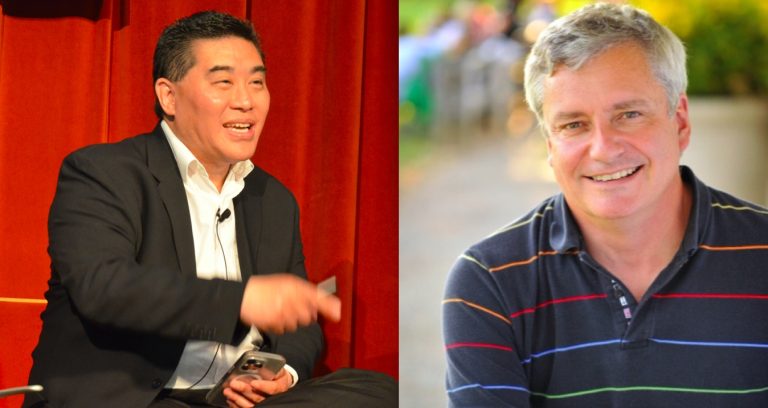
“We are finally seeing results from all the years of research and investment, and from patients participating in (cancer) research,” said Dr. Ed Kim, an oncologist who works as physician-in-chief and senior vice president for City of Hope Orange County, a branch of the Duarte-based cancer research center.
Kim, like others who’ve been working in cancer research and treatment since the 1990s, described a series of changes – some profound, some subtle – that have hit his profession over the past two decades.
Some drugs once used only for patients with advanced cancers have been deemed safe and effective for more people, boosting survivor rates. Biomarker testing – a genetic-based science that can help link specific treatments to specific cancers – has improved mortality numbers even though its widespread use is fairly new. Even some procedures that have been around for decades – surgical removal, for instance – are being used in new ways.
Overall, Kim described an evolving world in which cancer treatment is shifting from something akin to a broad, impersonal war – the blunt use of chemicals and weapons against mysteriously raging cancer cells – into something more like a series of criminal investigations, with genetics and other evidence used to solve individual cases of cancer.
“It’s a new era,” he said.
Odds in your favor
Related Articles
Opinion: California man’s medically assisted death offers lessons for everyone
These are the states that rank highest and lowest for women’s health in new report
Shannen Doherty established a unique way of getting cancer news from her doctor
Fine, white hairs on your nose? Could indicate cancer, doctor warns
U.S. Rep. John Garamendi announces cancer diagnosis
Not every number in the CDC’s report is uplifting.
For example, even though the national cancer death rate has dropped steadily since 2000, the total number of cancer deaths has not, rising by about 10.5% during the period tracked by the CDC, slower than the 18.5% growth in population in that period. In 2022, about 609,000 Americans died of cancer, making it the nation’s No. 2 killer, just behind heart disease. (The CDC also notes that cancer data from 2020 through 2022 was less reliable because the pandemic prompted some people to delay cancer screenings, and the surge in COVID-19 deaths may have masked some possible cancer deaths. In 2020 and ’21, COVID-19 was the No. 3 killer in the country, behind heart disease and cancer.)
That uptick in the raw death count is partly about age and obesity. Since 2000, America’s median age has jumped about 10%, to 38.8 years. Also, during that time, the percentage of American adults who are considered obese has jumped from about 31% to 42%. Because cancer is more lethal for older people, and often more common for people struggling with their weight, those factors have offset some of the gains made by technologies and treatments and healthier behavior.
Another factor in cancer’s stubborn lethality is equity.
People with no health insurance still die a lot more frequently of cancer than do the people with insurance. And the CDC numbers reveal shocking differences in cancer death rates based on race, gender and geography; a Black man living in Mississippi is three times more likely to die of cancer than an Asian woman in California.
Also, during the period tracked by the CDC, a few cancers (liver, uterine, pancreatic) appear to have become more lethal, not less. And huge gains made in prostate cancer death rates from the mid-1990s through the early 2000s – a result of the emergence of prostate-specific antigen (PSA) testing – appear to have leveled off since about 2012.
And, critically, while the nation’s cancer death rate has fallen, the rate at which new cancers are diagnosed has been close to flat, declining just 4.7% between 2000 and 2019. That suggests gains in cancer treatment are having a bigger impact than the gains in cancer prevention.
Still, the report tells a story of broad, long-term improvement. Cancer death rates have dropped – and survivorship has gone up – in every U.S. state and territory during the period studied. What’s more, the pace of improvement appears to be accelerating; from 2015 through 2019 cancer death rates in the United States fell by about 2% a year, doubling the pace of improvements made during the late 1990s.
Oncologists say all those changes have led to a simple, fundamental shift in the way they – and their patients – view cancer.
“You’re more likely to survive cancer, today, than you are to die from it,” Kim said.
“That wasn’t always true.”
Tasha and Kathie and tech
One of the numbers pulled from the CDC report is 3 million.
That’s roughly how many more Americans are living today because of lower cancer death during the past two decades, according to estimates by the CDC, the American Cancer Society and others.
No single technology or discovery is responsible for that.
But at least two women, Champion and Kathie Simpson of Mission Viejo, can point to a single advancement –- the arrival of oncotype testing for breast cancer, in 2004 – as a key reason why they’re around to share their cancer stories and confident about their futures.
The so-called “onco test” tracks 21 genes, and it can help predict a patient’s odds of developing breast cancer or the odds of breast cancer returning.
For Champion, the onco test was part of a broader story about her family history and her own future. She said her mother, who survived breast cancer in the late 1990s, was found in 2015 to carry the BRHC gene, a discovery that meant Champion and her two sisters might be at much higher risk than average of developing breast cancer. Champion soon took a similar test and was told she had an 87% chance of developing breast cancer, odds similar to what doctors gave to one of her sisters.
From there, Champion, a mother of four, opted to undergo a double mastectomy as a way to stave off any future breast cancer. But during that procedure, doctors found and removed a cancerous tumor, something that hadn’t been detected during a mammogram Champion had taken just six months earlier.
Discovery of the tumor – which Champion said was deemed “triple negative,” meaning it was more likely to be lethal – led to three rounds of intense chemotherapy, a lot of prayer and many late-night phone calls with her sister, who was living through a similar experience.
“People really questioned that surgery,” Champion said. “We were accused of not having enough faith, or of wanting a free implant job.”
But she said the subsequent cancer diagnosis was “more motivation than vindication,” and that the experience had the unexpected side effect of making her more confident.
“The decision reinforced my faith, in God and in myself,” she said. “I’d heard that little voice tell me to get the surgery and I listened to it.
“I have tried to continue doing that ever since.”
For Simpson, 48, who survived a 2021 breast cancer diagnosis, the onco test has produced a personalized report with a number – 19 – printed in large, bold type. The number reflects several factors in her genetic makeup and her current medical status that, combined, predicts she’s 94% likely to never experience a breast cancer recurrence.
The report, the detailed forecast, and the lumpectomy Simpson underwent with no follow-up chemo, were not widely available to breast cancer patients as recently as 15 years ago.
“For me, being a worrier, not a warrior, I don’t know what I would have done without that number,” Simpson said. “Ninety-four percent is a good number.”
Like Champion, Simpson – armed with a positive cancer forecast and a new, “don’t sweat the small stuff” mindset – is more confident today than she was before cancer. Last year, she and a partner quit their long-running jobs to start a new business (Keepsakes by KJ) selling souvenirs from around the world.
“The hardest thing in my life was telling my daughter, who was 16 at the time, ‘I have cancer,’” Simpson said.
“After that, everything is easy.”
Cancer for the cure?
Cancer might be the most well-funded issue in American life.
Politics, religion, even many other diseases can be divisive in some way. But raising money for cancer research and cures and prevention has been an ongoing part of American life since 1971, when then-President Richard Nixon signed the National Cancer Act.
Nixon’s idea was to use the space race template to focus the government on curing cancer. He even used the words “war on cancer” during the signing ceremony.
That effort didn’t quite pan out, but the mindset has carried on. Every president since Nixon has offered at least lip service to curing cancer. And cancer research, through the National Institutes of Health and other federal agencies, as well as the money generated by hugely profitable cancer drugs, has laid the foundation for many of the gains that are now bearing fruit.
It’s also why so many people, including Simpson, Champion and fellow cancer survivors Steve Bell of San Clemente and Michelle Rand of Hermosa Beach, spend at least some of their post-cancer lives promoting Relay for Life a series of walking/running events held in cities around the world that raise money for the American Cancer Society.
Rand, who in 2022 was diagnosed with an operable form of lung cancer – a version of the disease that wasn’t common even a decade ago, before improvements in surgical procedures and advances in lung cancer gene therapies – said the Hermosa Beach events she helps run have raised $4.1 million over the past 22 years.
She was raising money many years before she had cancer and says she plans to stay involved for many years to come.
“I’ve lost many friends to cancer over the years. But I’ve got a lot of friends who’ve lived, too. Now, that’s me.”
“I’m alive,” she added. “That’s my bottom line.”
Bell, who survived a 1997 bout with colon cancer, has spent most of his adult life helping that cause. The former manager for fitness and health programs in the city of Mission Viejo eventually became a full-time ambassador for the Relay for Life cause. That role has taken him to events around the country, as well as in Denmark, Gibraltar and Australia, among other places.
“Down there they call it bowel cancer,” Bell said, referencing the version of cancer he vanquished.
The fundraising, he said, is crucial.
“Of course, it matters,” he said. “There’s still so much to do.”
For Dr. Stephen Gruber, who directs the Center for Precision Medicine at City of Hope in Duarte, there’s just one thing on the to-do list: cure cancer.
“I use the word ‘cure’ as often as I can,” Gruber said.
“That’s because it’s true and appropriate. Many cancers are curable. We don’t use the word when we don’t have evidence, but the fact is that we are curing many more cancers than we used to. We’re not afraid of the word because we’ve made enough advances, and we’re in a situation of knowing the genomic profile of tumors that give us the power to use medication in very specific ways that, yes, lead to cures.”
“The future is bright,” Gruber added. “I’m incredibly optimistic.”