Corinne Purtill | (TNS) Los Angeles Times
As diagnoses of autism spectrum disorder have increased in the last two decades, so have the number of experimental and off-label therapies seeking to address the condition.
For parents navigating the complex and often contradictory landscape of autism interventions — while also balancing medical appointments, educational specialists and countless other family needs — evaluating these treatments can be daunting.
Experts in autism research talked to The Times about what parents and patients should watch for when evaluating a potential new treatment — for autism or any other condition.
Take testimonials with a grain of salt
Firsthand accounts of a therapy’s life-changing effects can be powerfully compelling. But such stories alone can’t indicate how effective a treatment will be for anyone else, autism experts said.
“Be wary of therapies that are sold to you with testimonials. If you go to a clinic website and they have dozens of quotes from parents saying ‘This changed my child’s life in XYZ ways,’ that isn’t the same as evidence,” said Zoe Gross of the Autistic Self Advocacy Network, a nonprofit group run by and for autistic adults. “If the main way something’s advertised is through testimonials, it may be because there isn’t research, or what research was done showed it wasn’t effective.”
Without accompanying data, there is no way to know whether any patient’s experience with a treatment is typical or an outlier. A therapy could have only a 1% success rate, Gross said, and still yield dozens of positive outcomes once thousands of people have tried it.
Former patient stories can be a starting point for an exploration of whether a therapy is right for someone, doctors said, but the exploration shouldn’t end there.
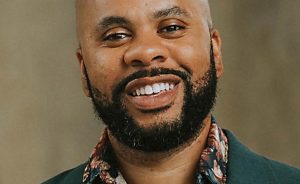
“There’s an old saying in medicine,” said Dr. Andrew Leuchter, director of UCLA’s TMS Clinical and Research Service. “The plural of anecdote is not data.”
Look for — and at — the research
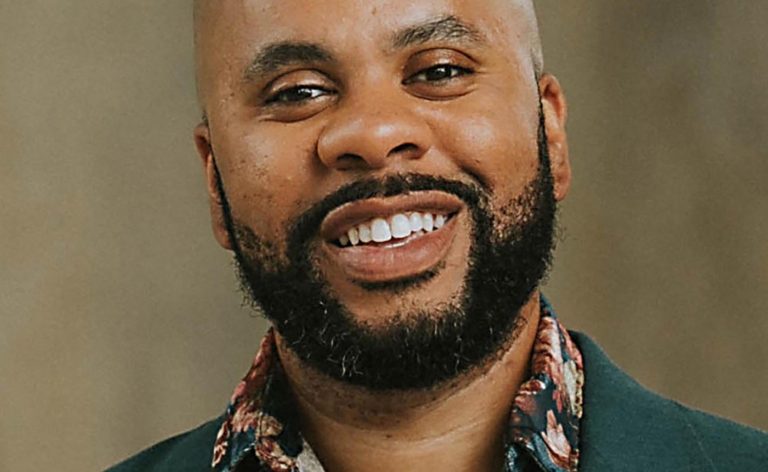
“Right now, it’s really sexy to call yourself ‘evidence-based,’” said Dr. David Celiberti, executive director of the nonprofit Assn. for Science in Autism Treatment. “For a consumer, that’s amazing. You hear ‘evidence-based’ and of course, you’re going to be drawn to it. But people are using that term very loosely.”
In the case of magnetic e-resonance therapy, or MERT, its developer Wave Neuroscience features on its website a library of research. Similar links feature on the sites of many licensee clinics.
Most of the publications related to autism cited by MERT clinics — and, at times, by Wave — are either limited in scope or only tangentially related to the therapy, a half-dozen experts said, including some whose work is cited.
One of them, for example, is a brief 2016 article from the Austin Journal of Autism and Related Disabilities titled “The Potential of Magnetic Resonant Therapy in Children with Autism Spectrum Disorder.”
Its authors and advisors said they were surprised to learn the paper was being used to advertise the treatment. The paper contains no data or original research and concludes only that MERT could be studied further as an autism therapy without risk of serious harm.
“This isn’t an evidence-based paper. It’s an opinion piece about the possibilities of this technology,” said Dr. John Crawford, a neurologist at Children’s Hospital of Orange County and a co-author of the paper. “It’s not that impactful from a scientific perspective.”
Who else has verified these findings?
Many MERT clinics feature a 2014 electronic poster presentation that examines data from the charts of 141 children who received transcranial magnetic stimulation, the therapy on which MERT is based, for autism.
Until March, Wave featured the poster on its website and highlighted that 59.1% of 44 participants who completed 12 months of treatment improved their scores on the Childhood Autism Rating Scale, an assessment tool used to gauge symptom severity.
A closer look at the report shows that after five days of treatment, 38 patients were dropped from the analysis because their symptoms either showed no improvement or worsened. One had a seizure during treatment.
The authors excluded dozens more patients for various reasons. Of the remaining 44 patients, 26 saw improvement while getting the treatment. That was 59.1% of those remaining, as the poster said, but only 18.4% of the total study population.
The write-up also notes that many of those 26 children were receiving other therapies at the same time that may have been responsible for some or all of the improvements.
Posters are typically prepared as a way to highlight findings at professional conferences and “cannot be interpreted as having undergone rigorous peer review,” said USC neurosurgeon Dr. Charles Liu, a co-author on the poster who is not affiliated with Wave or any MERT clinics.
“The main point of the abstract is and remains that more rigorous studies must [be] done.”
If research shows changes, how do you know the therapy caused it?
Wave and licensees also highlight a 2022 paper by a technician at a licensee clinic in Australia who is also a doctoral candidate at Australia’s University of the Sunshine Coast.
It looks at data from 28 patients at two MERT clinics in Australia whose brains showed “significant improvement” in their individual alpha frequency waves after treatment.
Although some previous research has found correlations between atypical alpha wave frequency and autism diagnoses, six scientists told The Times that there isn’t yet enough evidence to understand how changes in alpha waves affect autistic traits, or any scientific consensus on whether “improvement” in this pattern of brain activity has any meaningful effect on autistic behaviors.
The report is a retrospective chart review, which examines existing data from patients’ medical records and is often used to identify interesting outcomes worthy of further study.
By design it does not include a control group, which is what allows researchers to identify whether any changes they see are related to the variable they are studying. Its authors noted in the paper that findings are preliminary and require further study.
“Because this was not a controlled trial or study, [the cause of the changes] could have been anything including placebo effect, any additional therapies the children were receiving, etc.,” said Lindsay Oberman, director of the Neurostimulation Research Program at the National Institute of Mental Health.
Medical research follows a hierarchy of evidence. At the bottom are anecdotes and observations: valid points of information that alone aren’t enough to draw broad conclusions from.
Above that are observational studies that collect and analyze preexisting data in a systematic way. And at the top are randomized controlled trials, which are designed to eliminate as much bias as possible from the experiment and ensure that the thing being studied is responsible for any changes observed.
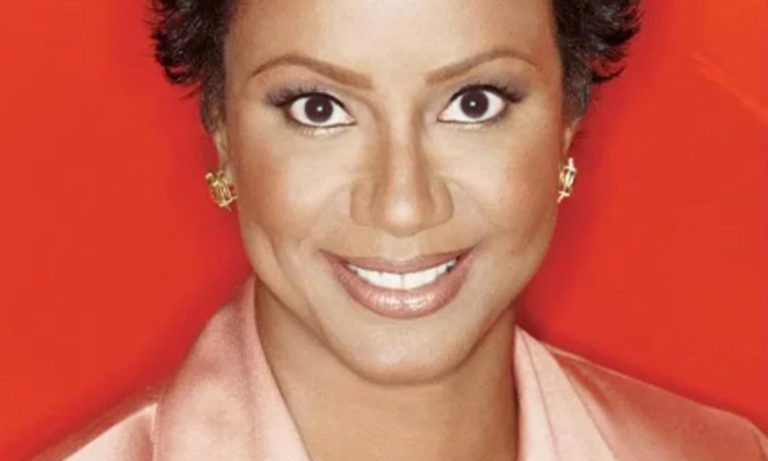
“Families need to know that there is this gold standard for studies — to make sure that something works to help people with autism, it needs to have what’s called a randomized controlled trial,” said Alycia Halladay, chief science officer at the Autism Science Foundation.
©2024 Los Angeles Times. Visit at latimes.com. Distributed by Tribune Content Agency, LLC.