Aaron Bolton, MTPR | KFF Health News (TNS)
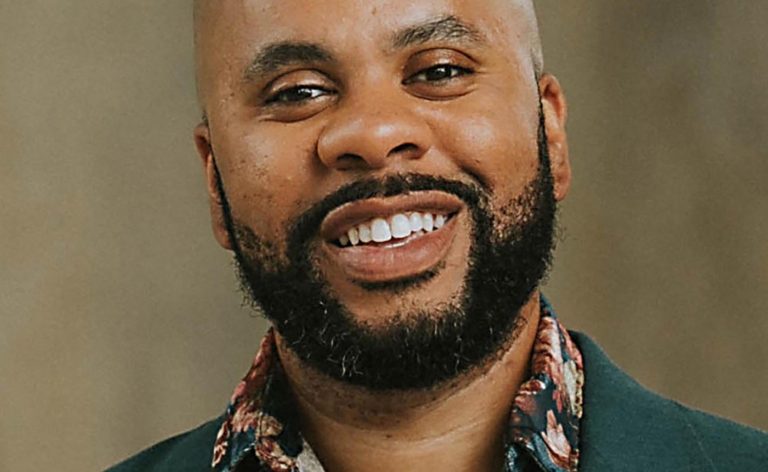
KALISPELL, Mont. — On a cold February morning at the Flathead Warming Center, Tashya Evans waited for help with her Medicaid application as others at the shelter got ready for the day in this northwestern Montana city.
Evans said she lost Medicaid coverage in September because she hadn’t received paperwork after moving from Great Falls, Montana. She has had to forgo the blood pressure medication she can no longer pay for since losing coverage. She has also had to put off needed dental work.
“The teeth broke off. My gums hurt. There’s some times where I’m not feeling good, I don’t want to eat,” she said.
Evans is one of about 130,000 Montanans who have lost Medicaid coverage as the state reevaluates everyone’s eligibility following a pause in disenrollments during the COVID-19 pandemic. About two-thirds of those who were kicked off state Medicaid rolls lost coverage for technical reasons, such as incorrectly filling out paperwork. That’s one of the highest procedural disenrollment rates in the nation, according to a KFF analysis.
Even unsheltered people like Evans are losing their coverage, despite state officials saying they would automatically renew people who should still qualify by using Social Security and disability data.
As other guests filtered out of the shelter that February morning, Evans sat down in a spare office with an application counselor from Greater Valley Health Clinic, which serves much of the homeless population here, and recounted her struggle to reenroll.
She said that she had asked for help at the state public assistance office, but that the staff didn’t have time to answer her questions about which forms she needed to fill out or to walk her through the paperwork. She tried the state’s help line, but couldn’t get through.
“You just get to the point where you’re like, ‘I’m frustrated right now. I just have other things that are more important, and let’s not deal with it,’” she said.
Evans has a job and spends her free time finding a place to sleep since she doesn’t have housing. Waiting on the phone most of the day isn’t feasible.
Tashya Evans waits outside the Flathead Warming Center, a low-barrier shelter in Kalispell, Montana, on March 5, 2024. Evans had just finished work in time to join the line for a bed that evening. (Aaron Bolton/MTPR/TNS) Joan Morris/Bay Area News Group
There’s no public data on how many unhoused people in Montana or nationwide have lost Medicaid, but homeless service providers and experts say it’s a big problem.
Those assisting unsheltered people who have lost coverage say they spend much of their time helping people contact the Montana Medicaid office. Sorting through paperwork mistakes is also a headache, said Crystal Baker, a case manager at HRDC, a homeless shelter in Bozeman.
“We’re getting mail that’s like, ‘Oh, this needs to be turned in by this date,’ and that’s already two weeks past. So, now we have to start the process all over again,” she said. “Now, they have to wait two to three months without insurance.”
Montana health officials told NPR and KFF Health News in a statement that they provided training to help homeless service agencies prepare their clients for redetermination.
Federal health officials have warned Montana and some other conservative states against disenrolling high rates of people for technicalities, also known as procedural disenrollment. They also warned states about unreasonable barriers to accessing help, such as long hold times on help lines. The Centers for Medicare & Medicaid Services said if states don’t reduce the rate of procedural disenrollments, the agency could force them to halt their redetermination process altogether. So far, CMS hasn’t taken that step.
Charlie Brereton, the director of the Montana health department, resisted calls from Democratic state lawmakers to pause the redetermination process. Redetermination ended in January, four months ahead of the federal deadline.
“I’m confident in our redetermination process,” Brereton told lawmakers in December. “I do believe that many of the Medicaid members who’ve been disenrolled were disenrolled correctly.
Health industry observers say that both liberal-leaning and conservative-leaning states are kicking homeless people off their rolls and that the redetermination process has been chaotic everywhere. Because of the barriers that unsheltered people face, it’s easy for them to fall through the cracks.
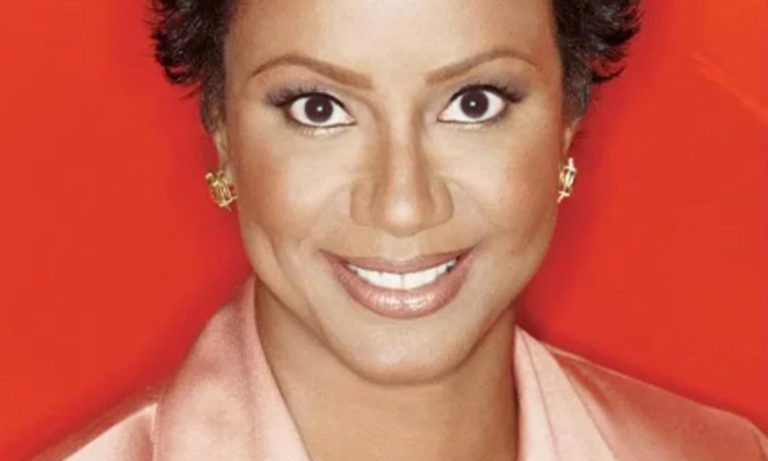
Margot Kushel, a physician and a homeless researcher at the University of California-San Francisco, said it may not seem like a big deal to fill out paperwork. But, she said, “put yourself in the position of an elder experiencing homelessness,” especially those without access to a computer, phone, or car.
If they still qualify, people can usually get their Medicaid coverage renewed — eventually — and it may reimburse patients retroactively for care received while they were unenrolled.
Kushel said being without Medicaid for any period can be particularly dangerous for people who are homeless. This population tends to have high rates of chronic health conditions.
“Being out of your asthma medicine for three days can be life-threatening. If you have high blood pressure and you suddenly stop your medicine, your blood pressure shoots up, and your risk of having a heart attack goes way up,” she said.
When people don’t understand why they’re losing coverage or how to get it back, that erodes their trust in the medical system, Kushel said.
Evans, the homeless woman, was able to get help with her application and is likely to regain coverage.
Related Articles
California is joining with a New Jersey company to buy a generic opioid overdose reversal drug
Kaiser Permanente may have sent private patient data to Google, Microsoft and X
CDC says it’s identified 1st documented cases of HIV transmitted through cosmetic needles
Biden administration shelves ban on menthol cigarettes
Holdout states consider expanding Medicaid — with work requirements
Agencies that serve unhoused people said it could take years to get everyone who lost coverage back on Medicaid. They worry that those who go without coverage will resort to using the emergency room rather than managing their health conditions proactively.
Baker, the case manager at the Bozeman shelter, set up several callbacks from the state Medicaid office for one client. The state needed to interview him to make sure he still qualified, but the state never called.
“He waited all day long. By the fifth time, it was so stressful for him, he just gave up,” she said.
That client ended up leaving the Bozeman area before Baker could convince him it was worth trying to regain Medicaid.
Baker worries his poor health will catch up with him before he decides to try again.
(KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs of KFF — the independent source for health policy research, polling and journalism.)
©2024 KFF Health News. Distributed by Tribune Content Agency, LLC.