Harnessing the body’s own cells to fight disease, long a medical dream, is finally a reality.
Now comes the bill.
Last month, Stanford became the first hospital in the nation to use a new $515,000 cell therapy to treat a patient with advanced melanoma. A related approach, costing $420,000 to $475,000, is offering hope to patients with lethal blood cancers.
Meanwhile, cells fixed by gene therapy can slow, even stop, the progression of intractable diseases like sickle cell or beta thalassemia — for the extraordinary price of $2.1 million to $4.25 million each.
Stanford cell therapy technologist Thomas Orozco thaws the treated immune cells from a patient with advanced melanoma. The cells are collected from the patient’s tumor and fortified in a laboratory to better fight the cancer. Photo provided by Stanford Health CareCell therapy technologist Thomas Orozco thaws the treated immune cells from a patient with advanced melanoma. The cells are collected from the patient’s tumor and fortified in a laboratory to better fight the cancer.[/caption]
This is the future of medicine, experts agree. But the cost of this new class of medical treatment is raising alarm about availability and affordability, even as its potential grows.
“Cell and gene therapies have the possibility to transform thousands of lives but only if we ensure sustainable access to them for all patients,” said Sarah Emond, president of the influential Institute for Clinical and Economic Review, a Boston-based nonprofit that assesses the value of medicines.
The prices aren’t yet unmanageable, because so few people are currently treated. Patients must travel to designated treatment centers, and they aren’t being referred by community physicians. But referrals and demand should increase as more treatments are introduced that serve a wider population.
Most health insurers in the United States aren’t set up to support one-time personal therapies that deliver long-term benefits, at unprecedented prices.
“These are precision medicines,” said Dr. David Miklos, chief of the Stanford Bone Marrow and Cell Therapy Program, where hundreds of cancer patients have been treated with the CAR-T cell therapies. “It’s different than buying a pill at the CVS pharmacy that can work for anybody.”
The promise of cell and gene therapies has intrigued scientists for decades, but progress was slow, with many setbacks. Now the long research journey has finally paid off, with FDA-approved products entering the clinic.
“The technology to bring it to life has finally caught up with the ideas behind it,” said Stanford assistant professor of medicine Dr. Allison Betof Warner, who is conducting Stanford’s melanoma trial.
Cell-based strategies are delivering the most celebrated cancer treatments to emerge in decades.
In one approach, called chimeric antigen receptor (CAR) T-cell therapy, patients’ immune cells are collected and genetically modified to better fight lymphoma, leukemia, and, most recently, multiple myeloma.
Another uses a different approach, enlisting tumor-infiltrating lymphocytes, or TILs. These immune cells are harvested from the tumor, fortified in the lab and then returned to the patient. In clinical trials, about 30% of patients had their incurable melanoma tumors shrink or disappear.
“I’m very happy that it’s here now. … I’ve been walking the tightrope and I didn’t fall off,” said a Stanford patient, who asked not to be identified.
Gene therapy also uses engineered cells, with genes replaced, deleted or inserted. On Wednesday, Kendric Cromer, a 12-year-old boy from a suburb of Washington, D.C., became the first person in the world with sickle cell disease to begin an FDA-approved gene therapy. Stanford and UCSF will both offer this treatment.
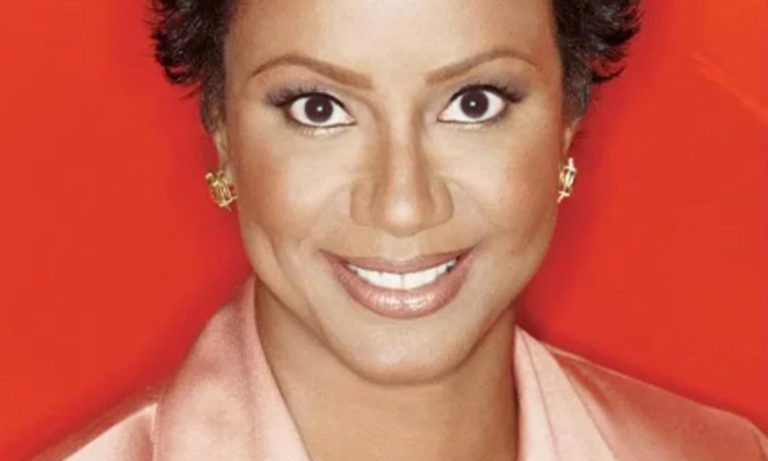
Dr. Allison Betof Warner of Stanford Health Care provided a new cell-based therapy for a patient, who asked not to be identified, with metastatic melanoma. The one-time treatment, which costs $515,000, uses immune cells harvested from the patient’s tumor. Photo provided by Stanford Health Care
Scientists are now working to expand the therapies’ repertoire to attack solid tumors, autoimmune diseases, aging, HIV and more.
“It’s just the beginning of a new era,” said biochemist Wendell Lim, director of the UC San Francisco Cell Design Institute.
“It shows that we can take a living cell and change what it does, so it makes new sorts of decisions and carries out complex actions. It processes information, like a little computer,” he said. “This is very different from a static thing, like a chemical.”
It’s still early, and few patients are taking advantage of these new groundbreaking therapies, said physicians.
Why? Word hasn’t yet gotten out, so sick people aren’t getting referred from their community physicians, said Miklos. Treatment is risky. Or patients may live far away from the nation’s estimated 30 “centers of excellence,” like Stanford and UCSF, and are daunted by the cost of travel and housing.
Payment isn’t guaranteed; it’s decided on a case-by-case basis. Medicare and MediCal cover the cost of care when it is determined to be medically necessary. So does Kaiser.
The great majority of private insurers cover treatments, although sometimes back-and-forth negotiations are needed, said Gary Goldstein, who oversees the business operations of Stanford’s Blood & Marrow Transplant Program.
The sticker price just covers parts — no labor, no warranty. Drug prices aren’t regulated, like utilities, and there is no cap on what a company can charge.
The total cost for gene therapies over the next decade has been estimated to reach an eye-popping $35 billion to $40 billion. The bill for future cell therapies, which could help a bigger pool of patients, will likely be higher.
Drug makers argue that the prices reflect the powerful clinical benefit and the risks and uncertainties of development. A one-time therapy for a chronic condition may actually save money, they add, by sparing a lifetime of care.
“We’ve never cured patients with a single treatment before,” said UCSF’s Dr. Greg Allen, who is designing immune cell therapies for notoriously difficult-to-treat tumors, like those of the pancreas and lung. “So it’s very exciting.”
For some patients, it may be their last best chance.
“I don’t think there’s a price on a life,” said Stanford’s Betof Warner. “These are patients who don’t have another option.”
If millions of people are helped, as hoped, it will create budget pressures on the federal government and larger payers, while smaller employers, state Medicaid plans, and regional health plans may find providing access financially impossible, warn economists. Health care costs are already outpacing inflation, climbing 7% this year.
“It’s going to put a lot of stress on the system,” said Edwin Park at the Georgetown University McCourt School of Public Policy. “But the issue is critical because you don’t want the high price of these therapies to result in low-income people not being able to access them.”
Already, governments and commercial insurers are scrutinizing treatments’ effectiveness. Some are imposing strict restrictions on who is eligible. They’re asking manufacturers for discounts and rebates.
Related Articles
Our brains are growing. Will that help prevent dementia?
California strikes deal for cheaper overdose-reversing medication
California is joining with a New Jersey company to buy a generic opioid overdose reversal drug
Dozens of deaths reveal risks of injecting sedatives into people restrained by police
Bird flu’s disturbing new turn into cattle — are California herds safe?
Scientific advances could cut costs, said Lim. One idea is to design cells that are immunologically universal, so that a single source could treat many patients. Another is to build a large “cell bank” of precursor stem cells. A third is to ask the body to do its own manufacturing, by introducing an engineered virus that can fix cells.
If manufacturing is localized — making the cells at Stanford or UCSF, for instance, rather than at distant drug companies — that would bring costs down, said Miklos.
As competition grows, prices will fall, he predicted.
Meanwhile, the health care system must focus on finding innovative payment solutions, said Emond.
One proposal is to amortize how much insurers pay over time, like a home mortgage. Another is for drug companies to provide a prorated refund if a patient doesn’t improve — a “pay for performance” model. Yet another option would be a subscription-based approach, like Netflix, where insurers shell out a monthly fee to access however much therapy is needed.
“As we look to the future,” said Emond, “this is a moment where we can discuss how to do things differently.”